Medicaid Capitated Payment Reconciliation
Recapture Lost Revenue
Automate Your Medicaid Capitated Payment Reconciliation
Medicaid MCOs may be leaving millions of dollars in capitated payments on the table due to manual or poor reconciliation processes.
Certifi can help ensure the accuracy of every Medicaid capitated payment you receive. We ingest enrollment and biographic information, rate determinants and payment files. Then, we apply rate rules to coverage information and generate expected payment transactions. Finally, we apply payment transactions to expected transactions to generate a variance report that highlights payment discrepancies.
Our solution automates capitated payment reconciliation, potentially recapturing millions of dollars annually. Plus, our Perfect Balance™ design couples debits and credits, improving the accuracy of payment calculations in high retroactivity environments like Medicaid.
Automate Reconciliation. Save Money.

Recapture Lost Revenue
Leverage enrollment and payment data to automate reconciliation by comparing actual capitated payments to expected payments.
Automate Retroactivity
The constantly changing status of beneficiaries leads to increased retroactivity. Our Perfect Balance™ design simplifies retroactivity management.
Track Payments and Discrepancies
From variance reports to accounts receivable aging reports to general ledger exports, we make it easy to track payments and discrepancies.
Medicaid Payment Reconciliation
Integrate
Certifi integrates with enrollment platforms and ingests payment data to streamline the reconciliation process.
Automate
Automate reconciliation and ensure the accuracy of every capitated payment.
Reconcile
Compare expected payment transactions to actual payments to pinpoint any variations.
Report
Generate variance reports, accounts receivable aging reports, general ledger files for premiums received and more.
You could be losing millions of dollars every year through poor manual reconciliation. Learn how to automate your Medicaid payment reconciliation and recapture lost money.
Easy to Implement. Instant ROI.
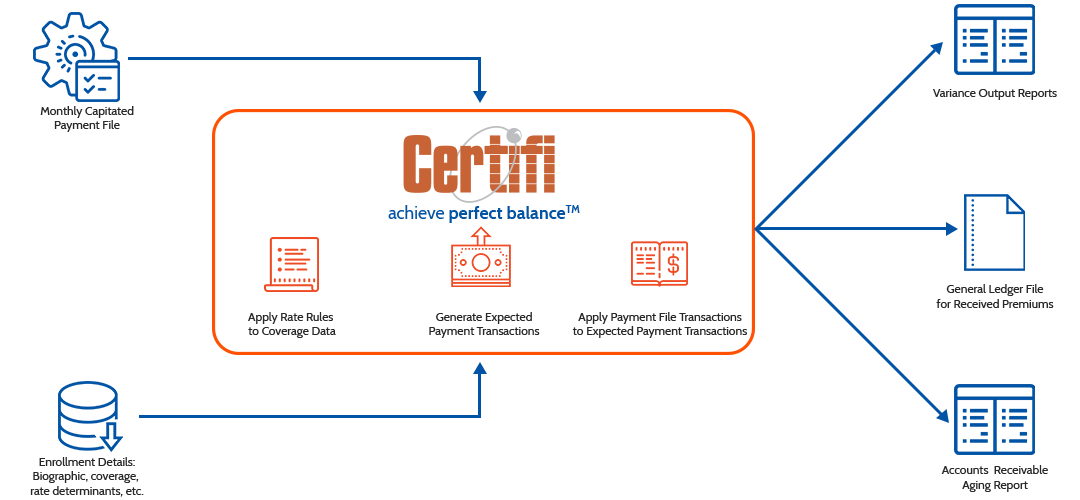
Certifi simplifies Medicaid Capitated Payment Reconciliation. We ingest enrollment, coverage, and rate data, then apply rate rules to coverage information to generate expected payment transactions. Those expected payment transactions are compared to actual payments to discover discrepancies. We then generate variance reports to help you understand any payment discrepancies, as well as general ledger files for received premiums and accounts receivable aging reports.
Seeing is Believing.
Complete the form below and we’ll call you to schedule a demo of Certifi’s Medicaid Capitated Payment Reconciliation.
"*" indicates required fields

