In early 2023 the top U.S. health insurers released their 2022 end-of-year financial results. Overall, revenues were up, several large acquisitions were completed, profits varied and rebrands and realignment flourished. Learn more about 2022 health insurer financial results and key corporate activities:
Humana
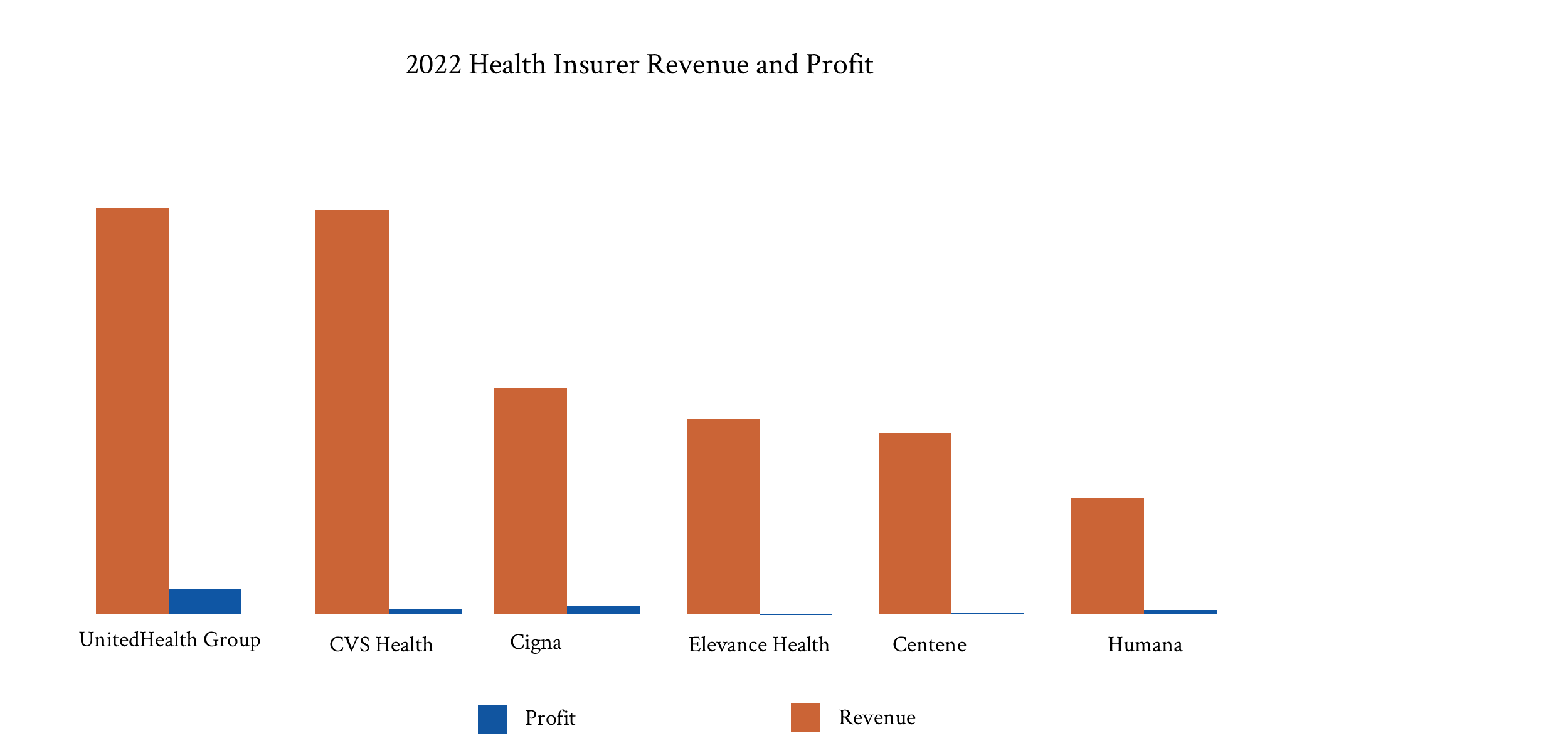
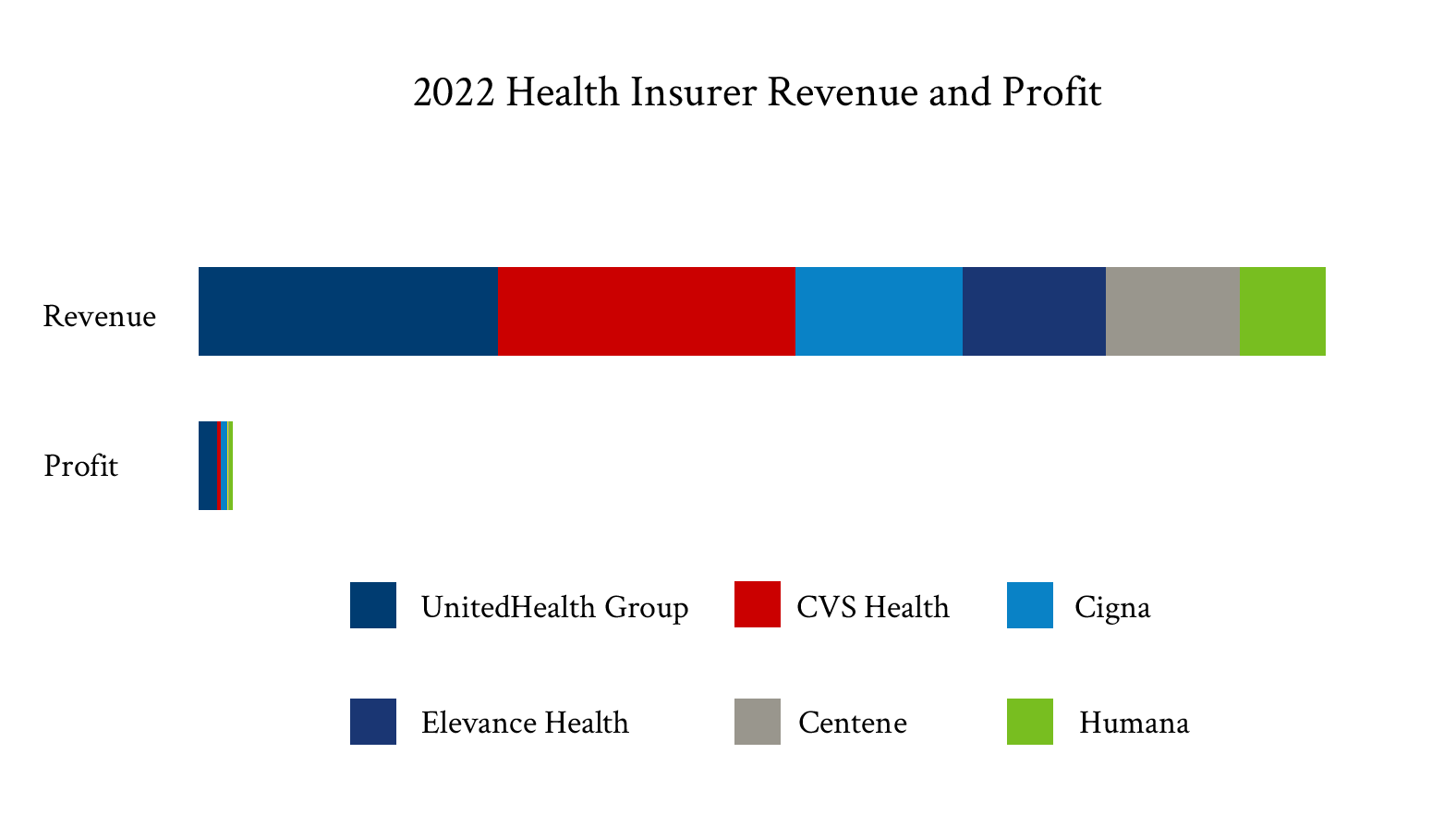
Revenue: $93 billion
Profits: $3.5 billion
Humana reported strong revenue growth in 2022, earning nearly $93 billion, up from just over $83 billion in 2021. Profits were up $200 million from 2021 to just over $3.5 billion.
Realignment
Like other large health insurers, Humana announced a realignment, creating two segments within the organization. One, aptly named Insurance, will focus on the company’s insurance products, including its pharmacy benefit management. The other segment, CenterWell, will focus on healthcare services like pharmacy dispensing, and provider and home services.
After announcing its 2022 financial results, Humana also announced that it would be exiting most group markets, instead focusing heavily on Medicare Advantage plans. That exit and Humana’s investments in scaling its senior-focused primary care clinics and Kindred at Home acquisition have positioned the company well for Medicare Advantage growth.
2023 Outlook
After disappointing Medicare Advantage growth in 2021, Humana performed much better during the 2023 open enrollment period, adding at least 625,000 members. Humana expects that growth to be higher than the industry average. As a result, Humana indicated it was on track to hit its 2025 adjusted earnings per share target of $37. It reported a $25 adjusted EPS in 2022.
Cigna
Revenue: $180.5 billion
Profits: $6.7 billion
Cigna, a global health services company, reported revenue of $180.5 billion in 2022, including profits of $6.7 billion. Revenue increased by almost $6.5 billion in 2022, while profits grew by nearly $1.5 billion.
Branding
In February, Cigna launched a rebrand. The overall business will now be named the Cigna Group. Brands underneath that group include Cigna Healthcare, the company’s U.S. and international commercial and government plans, and Evernorth Health Services, the company’s pharmacy benefit management, data analytics, and care-delivering solutions.
Sales Activity
In 2022 Cigna also sold business units. The company completed the sale in July of its life, accident, and supplemental business in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan, and Thailand to Chubb for $5.75 billion. In January it completed the sale of its Texas Medicaid business to Molina for $60 million.
2023 Outlook
Cigna expects 2023 revenue to grow to $187 billion. It expects adjusted profits near $7.33 billion.
UnitedHealth Group
Revenue: $324.2 billion
Profits: $20.1 billion
A behemoth in the healthcare industry, UnitedHealth Group reported a 13% year-over-year revenue increase, remarkable considering revenues of $324.2 billion in 2022. Even more notable relative to its peers: UnitedHealth Group experienced profits above $20 billion in 2022.
Acquisitions
Most significantly, UnitedHealth completed its $13 billion acquisition of Change Healthcare in late 2022 after a federal judge cleared the way for the acquisition. The deal merges the healthcare data and analytics organization with Optum Insight. The company also purchased LHC Group for $5.4 billion to beef up its home health capabilities.
Other acquisitions were less high profile, including acquiring care providers like Refresh Mental Health, Atrius Health, and Kelsey-Seybold Clinic. It also purchased KS Plan Administrators, a Medicare insurer based in Houston.
2023 Outlook
UnitedHealth Group expects double-digit revenue growth to continue in 2023, projecting revenue to be between $357 billion and $360 billion. Profits will continue to be strong, with profit expectations between $21.7 billion and $22.3 billion in 2023.
CVS Health
Revenue: $322.5 billion
Profits: $4.1 billion
CVS Health reported a 10.4% revenue increase in 2022, with total revenue just below UnitedHealth Group at $322.5 billion. Profits were $4.1 billion, down from 2021’s $7.9 billion.
Acquisitions
Like other large health insurers, CVS isn’t afraid to make significant acquisitions that fit its strategic goals. In 2022, it purchased Signify Health, a company leveraging analytics and technology to help manage in-home care, for nearly $8 billion. In 2023, the company announced plans to buy Oak Street Health, a value-based primary care provider, for over $10 billion.
Divestitures
The company also netted nearly half a billion dollars by selling benefits technology company bswift and health savings account provider PayFlex in separate deals.
2023 Outlook
CVS Health expects revenue to grow in 2023 to between $332.7 and $338.5 billion, representing 3% to 5% growth.
Centene
Revenue: $144.5 billion
Profits: $1.2 billion
Centene reported 15% revenue growth for 2022 totaling $144.5 billion. Profits reached $1.2 billion. The company’s revenue growth was primarily attributed to Medicaid membership expansion, up nearly 1 million from 2021, thanks to the temporary suspension of redeterminations during COVID-19. Medicare Advantage membership also grew by just over 250,000 lives.
Divestitures
Centene also divested itself of numerous business units in 2022. After purchasing Magellan Health in 2022, Centene sold off Magellan RX to Prime Therapeutics for $1.5 billion. The company also sold Magellan Specialty Health to Evolent Health for over $750 million. It also completed the sale of Ribera Salud, a healthcare provider in Spain, to Vivalto Sante, Centurion Health, a prison healthcare provider, to an unknown buyer, and HealthSmart, a home healthcare supplemental benefits company, to Convey Health Solutions.
2023 Outlook
Like other insurers, Centene increased guidance for 2023, expecting an additional $2 billion in revenue thanks to a change in its expectations for when Medicaid redeterminations will occur and a higher enrollment starting point and higher than expected Marketplace enrollment. Centene expects revenue to be between $131.5 and $133.5 billion.
Elevance Health
Revenue: $155.7 billion
Profits: $949 million
Elevance Health experienced a nearly 14% revenue growth in 2022, up to $155.7 billion. Profits were just under $1 billion, down 16.5% year-over-year.
Rebrand
Like other insurers, Elevance Health underwent a rebrand. The company changed its corporate brand from Anthem to Elevance. Additionally, it introduced a new brand, Carelon, for its healthcare services unit. Finally, it resurrected its Wellpoint brand – its corporate brand until 2014 – for some government-subsidized insurance products.
Acquisitions
Elevance also recently announced that it would acquire Blue Cross Blue Shield of Louisiana for at least $2.5 billion. The deal, expected to close by the end of 2023, will bring about 1.6 million members and $4.5 billion in revenue to Elevance.
Elevance also closed its deal with BioPlus, a specialty pharmacy that helps deliver services for patients with chronic conditions like cancer, multiple sclerosis, autoimmune diseases, and rheumatology.
2023 Outlook
Elevance expects revenue of $164 billion in 2023 and expects its total membership to grow by roughly half a million lives and settle somewhere between 47.4 million and 48.5 million, with most market segments – commercial, individual, and Medicare Advantage – growing while Medicaid enrollment declines as a result of the resumption of redeterminations in April.
Certifi’s health insurance premium billing and payment solutions help healthcare payers improve member engagement while reducing administrative costs.